"There is nothing so practical as a good theory."
Kurt Lewin (?)
I can't resist commenting on Daphne Merkin's New York Times article on her (mis)adventures in therapy, not specifically because of its implications for her or for psychoanalysis, but because of general issues it brings to mind regarding diagnosis and levels of understanding.
On a human level the piece intrigues mainly with its idiosyncratic portraits of Merkin's successive therapists; taking full advantage of the writer's prerogative, she turns the tables by pigeonholing them (this one is dowdy, this one seedy, this one aloof, etc.) just as they would aspire to pigeonhole her. However, the surprising yet perhaps telling thing is that she doesn't actually document them pigeonholing her, that is, there is almost no discussion of diagnosis beyond the vaguest of terms: anxiety, depression, neurosis.
It is not my role her to speculate on Daphne Merkin, who is a brilliant writer. But any decent clinician is going to have one diagnosis come to mind when she discusses having poor boundaries, chaotic relationships, one therapist who comments on her difficulties with navigating emotional proximity, and at least one episode of severe regression when given free rein to explore her childhood issues. And yet there is no discussion of diagnosis or its extension, prognosis; that is, what pattern exists here and how might it unfold over time?
Merkin seems surprised herself at how little overall clinical effect her perpetual "life in therapy" has had, not least because while some of her therapists were clueless and unhelpful, others were deeply empathic and understanding. Indeed, she felt very understood by and very attached to at least a couple of them, and yet nothing seemed to change for her overall, at least in the way she was hoping for. What is going on here?
This question also came to mind when I read Cheryl Fuller's most recent post on obesity which, while making no explicit reference, followed and seemed an implicit response to my most recent post here. Her eloquent post, decrying allegedly simplistic overgeneralizations, was a plea for deep understanding of the individual experience of obesity. It brought to mind what I see as a tension between empathy and theory (or diagnosis) as ways of knowing that have different but complementary purposes.
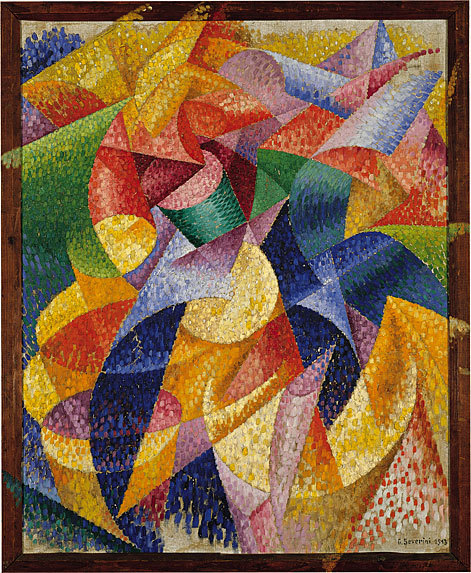
Empathy is, of course, a fine-grained attunement to an individual's emotional state and history, an engagement with a truly unique sensibillity and life trajectory. This is obviously a form of knowledge, and may be likened to other forms of perception that are sui generis: a singular Picasso, or a sunset whose precise configuation of color and shadow will never be precisely repeated anywhere or at any time. Human beings have a powerful need to understand and to be understood in this way, which is the way of love, friendship, ethics, and aesthetics. It is what most people think of as the ends (i.e. the goals) of human life.
However, the whole point of theory and diagnosis is to overlook endless idiosyncratic differences and to identify how entities and processes may be alike, not how they differ. This kind of classification has three purposes: it enables us potentially to know how phenomena may develop over time, how we may go about modifying them, and on a more abstract level, how "it all fits together." The former two aims are those of science, while the latter aim belongs to spirituality. These things are necessary because a universe of irreducible uniqueness is also a universe of chaos (and also a universe without language, which also intrinsically glides over differences; a language could do full justice to individuality only if it had as many words as there are entities).
A good theory (or diagnosis in medicine) should either either lead to effective interventions or to a recognition of the necessary limits of treatment, i.e. prognosis. A theory that aids in neither altering nor predicting outcomes is useless. But there are different levels of explanation with corresponding different levels of treatment. For instance, we lack an ultimate theory of obesity, that is, an explanation of who gets fat and why, but we have a more proximate theory: obese people become obese because more energy is absorbed through their stomachs than their bodies expend as energy. Therefore one can intervene at that level of explanation through bariatric surgery (the ethical and cultural considerations of which I'm not touching here).
To come back around to Daphne Merkin's quandary: as presented in her article at least, the diagnostic/theoretical system has failed her on multiple levels. For while psychoanalysis has never been accused of neglecting theory, and the practices she describes imply a theory, this is never made explicit to her. While there may be passing and perceptive interpretations, no therapist ever comes out and says what may be wrong with her.
There is also a problem with prognosis. If I see someone who has seen a dozen other doctors over decades without success, then there are three possibilities (listed in ascending probability): the diagnosis is wrong, the diagnosis is right but not every possible treatment has been tried, or the condition is untreatable. Merkins's therapists never seem to consider that the diagnosis may be one that is not amenable to classical analysis. Or even if they consider this option but reject it, they are undeterred by the failure of a dozen of their colleagues in the past. Why? Perhaps because in psychoanalysis idiosyncrasy plays such a primary role that there are as many different treatments as there are individual therapists. The last option is that her therapists know that the treatment will not work in any conventional sense but view it as a kind of palliative care. This seems to be Merkin's own take on it; by the end she is not hopeful of any real progress, but life in therapy seems at least slightly less intolerable than life without.
So medicine and psychiatry need both levels of understanding: the empathic and the theoretical. If the latter unopposed is crude and callous, the former unopposed is static and ineffectual. Theory enables us to manipulate the world (including our own bodies) to our own ends, while empathy enables us to decide what those ends will be. When it comes to psychiatry, as I have written here in the past, flaws in treatment are far less grievous to the profession than flaws in diagnostic understanding. As perpetual debates over psychoanalysis and the DSM-5 demonstrate, our map of the human psyche still has wide swaths of empty space, offering limited guidance to those lost on the way. Our minds so often rush to treatment options (how do we get there from here?) that we often skip a crucial orientation step (where are we exactly?). Psychiatry will be waiting for its GPS for a long time. When we finally get it, let's not become overly dependent on it...
2 comments:
Could it be that some people just like therapy?
In Merkin's case, maybe perpetual therapy is not entirely unhealthful, even though not necessarily helpful. It's just a lifestyle choice. A point of anchorage. A space without the urgency of real time. There are worse habits/attachments/addictions.
Indeed, although it's unclear whether she could be said to "like" it in the way that someone "likes" to destress with a massage every now and then, or the way that a hypochondriac "likes" to haunt doctors' offices. I'm not implying she's a hypochondriac, but it's unclear whether it's a matter of preference or inner compulsion.
We don't know whether a prolonged absence from therapy is helpful or harmful in her case because it apparently hasn't been tried.
Post a Comment